Designing a Care Map
Review the medical conditions in the textbook, including osteoporosis, osteomyelitis, disorders of the feet, plantar fasciitis,
carpal tunnel disorder, rotator cuff injury, or other musculoskeletal disorders.
Develop a care map using this template.
In this table, include this information:
Relevant data: Disease process, common lab work and diagnostics, and subjective, objective, and health history data
Three NANDA-I approved nursing diagnoses
One SMART goal for each nursing diagnosis
Two nursing interventions provided with a supporting rationale for each SMART goal for a client with a musculoskeletal
disorder.
Two scholarly sources to support information in the care map.
Cite sources in-text and on a reference page using APA format.
Choose one for the designing a care map assignment.
- Ms. C.S. is a 76-year-old white female with osteoporosis, who presents to her
primary care physician for further work up after being seen and treated by an
orthopedic surgeon for a right distal radius fracture. Patient sustained a low
impact fall from standing which led to her injury. She states generally she doesn’t
have pain but rates pain in wrist seven out of ten on pain scale. Current
medications: Insulin pump with Lispro insulin 2 units per hour. Patient reports that
she doesn’t like to cook so skips lots of meals.
Past Medical and Surgical History
Bipolar disorder, diagnosed age 23, medically treated with lithium and
cognitive behavior therapy.
Hysterectomy, at age 44.
Diabetes type 1 diagnosed age 2.
Depression diagnosed age 17.
Social History
One pack per day smoker since age 17
Has recently been told by primary care physician she is underweight:
Height 5’2 weight 85 pounds. - A 10-year-old girl presents at the hospital with her parents, complaining about
pain of the left knee after an accident sustained during trampoline jumping. The
patient had a superficial skin abrasion but due to decreasing pain no doctor was
consulted. Three weeks later she walked 3 miles during a school trip causing
moderate pain of her left knee mainly during night-time. The pain was associated
with swelling and redness over the left knee. The family consulted a medical
practitioner. The patient was treated with NSAID (Motrin 100mg every 6-8 hours)
which the family is still regularly using. Due to persisting pain that patient rates as
8 out of 10, patient is here to be evaluated 8 weeks after the injury. Physical
examination revealed a painful leg extension, increased discomfort with walking
and palpitation of the patella. The erythrocyte sedimentation rate is 19 mm/h
(normal range: 1–10 mm/h) and WBC count is 15,500 cells/mm3 (normal range
for a 10-year-old: 4,800 to 10,800 cells/mm3). For further diagnostics,
radiograph and a subsequent MRI of the left knee were performed showing an
osteolytic lesion with a diameter of 1.5 cm of the patella with central necrosis.
Patients and patient report that no past medical history or surgeries. Currently
taking the Motrin for pain and a children’s multivitamin daily. Patient states, “I just
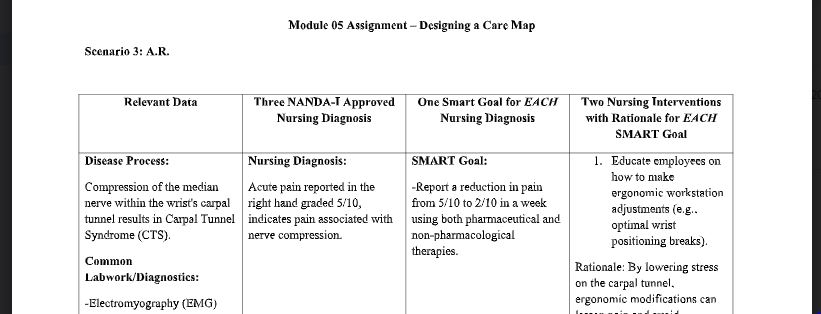
want to play soccer again with my friends, it hurts to much now.” - A.R. is a 45-year-old male that comes to the clinic for carpal tunnel assessment.
Patient states, “I have been feeling numbness, tingling, and pain in my right
hand with the first three digits of my hand involvement for the last 2 days.” The
discomfort gets exacerbated as he does repetitive computer work and gets mildly
relieved with handshaking and change of positions. A.R. rates his pain at a 5 out
of 10 with no radiation but is intermittent. A.R. has a desk job at a local insurance
company. He has been taking Tylenol 500mg every 6 hours when at work due to
pain is worse at work for the past 2 days with little symptom relief. Patient denies
any recent fall or trauma to the involved extremity. Denies any pat medical history
or surgeries. Reports no known allergies. Vital signs: Temp 98.3 F, HR 69, BP
111/76, RR 13, and O2 saturation 98%. Positive Tinel sign and Phalen test.
Positive paresthesia with numbing and tingling of right thumb, index and middle
finger with palmar, dorsal hand and forearm involvement. Thinner muscles at the
base of the thumb atrophy. No muscle weakness noted. - Karen a 32-year-old woman comes into the clinic. Chief complaint is
stabbing pain in the bottom of foot near the heel. Patient reports,
“Pain is usually the worst with the first few steps after awakening, but
it also triggered when at work.” Patient is a personal trainer. She
stands for long periods of time. Patient states, “I run 10 miles daily
and I notice that when I get home after a run the pain is also worse.”
Patient is currently taking Ibuprofen 400mg every 6 hours for the last
2 days. On exam the patient grimaces and flinches when pressure
applied to the bottom of her foot near the heal. The provider also
notes that the plantar fascia is very tight on the bottom of the foot
along with tissue inflammation in the arch of the foot. Patient does
stat that her hamstrings have also been unusually tight when running.
Patient reports that first thing in the morning when getting out of bed
the pain is an 8 out of 10 then as the day progresses the pain
reduces to a 4 out of 10. When she is running the pain goes to an 8
out of 10 again. Denies any chronic medical conditions or current
surgeries. Vital signs : HR- 72 RR- 18 BP – 110/68
Answer Preview for Designing a Care Map
APA
300 Words
